How is coronary artery disease diagnosed?
The resting electrocardiogram (EKG) is a recording of the electrical activity of the heart, and can demonstrate signs of oxygen starvation of the heart (ischemia) or heart attack. Often, the resting EKG is normal in patients with coronary artery disease and angina. Exercise treadmill tests are useful screening tests for patients with a moderate likelihood of significant coronary artery disease (CAD) and a normal resting EKG. These stress tests are about 60 to 70% accurate in diagnosing significant CAD.
If the stress tests do not reveal the diagnosis, greater accuracy can be achieved by adding a nuclear agent (thallium or Cardiolite) intravenously during stress tests. Addition of the nuclear imaging agent allows imaging of the blood flow to different regions of the heart, using an external camera. An area of the heart with reduced blood flow during exercise, but normal blood flow at rest, signifies significant artery narrowing in that region.
Combining echocardiography (ultrasound imaging of the heart muscle) with exercise stress testing (stress echocardiography) is also a very accurate technique to detect CAD. When a significant blockage exists, the heart muscle supplied by this artery does not contract as well as the rest of the heart muscle. Stress echocardiography and nuclear stress tests are both at least 80% to 85% accurate in detecting significant coronary artery disease.
Medicines used to treat angina reduce the heart muscle demand for oxygen in order to compensate for the reduced blood supply. Three commonly used classes of drugs are the nitrates, beta blockers and calcium blockers. Nitroglycerin (Nitro-Bid) is an example of a nitrate. Examples of beta blockers include propranolol (Inderal) and atenolol (Tenormin). Examples of calcium blockers include amlodopine and felodopine. Unstable angina is also treated with aspirin and the intravenous blood thinner heparin. Aspirin prevents clumping of platelets, while heparin prevents blood clotting on the surface of plaques in a critically narrowed artery. When patients continue to have angina despite maximum medications, or when significant ischemia still occurs with exercise testing, coronary arteriography is usually indicated. Data collected during coronary arteriography help doctors decide whether the patient should be considered for percutaneous coronary intervention, or percutaneous coronary intervention (PCI), whereby a small stent is used to open up the blockage.
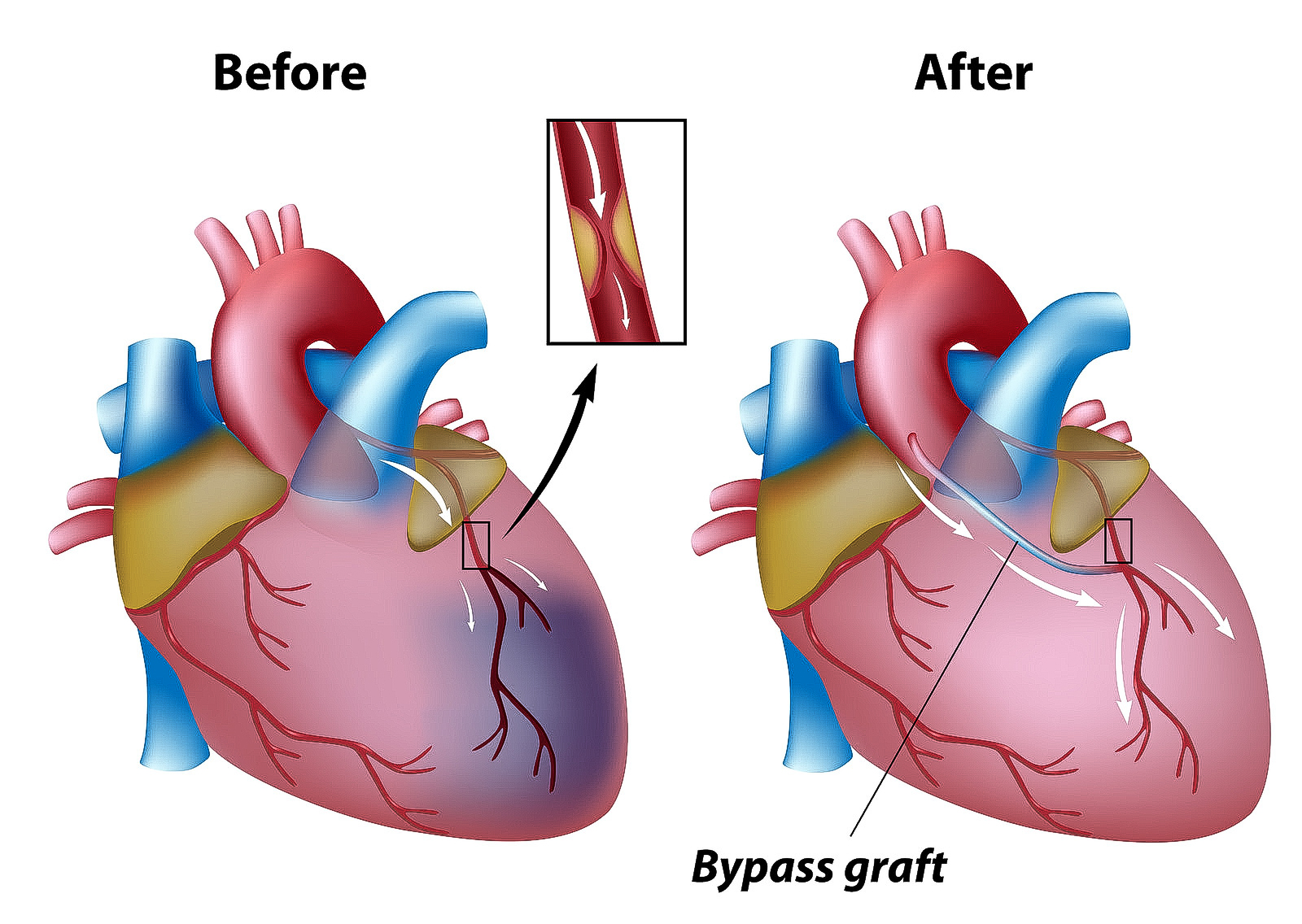
The cardiac surgeon makes an incision down the middle of the chest and then saws through the breastbone (sternum). This procedure is called a median (middle) sternotomy (cutting of the sternum). The heart is cooled with iced salt water, while a preservative solution is injected into the heart arteries. This process minimizes damage caused by reduced blood flow during surgery and is referred to as “cardioplegia.” Before bypass surgery can take place, a cardiopulmonary bypass must be established. Plastic tubes are placed in the right atrium to channel venous blood out of the body for passage through a plastic sheeting (membrane oxygenator) in the heart lung machine. The oxygenated blood is then returned to the body. The main aorta is clamped off (cross clamped) during CABG surgery to maintain a bloodless field and to allow bypasses to be connected to the aorta.
Sutures are removed from the chest prior to discharge and from the leg (if the saphenous vein is used) after 7 to 10 days. Even though smaller leg veins will take over the role of the saphenous vein, a certain degree of swelling (edema) in the affected ankle is common. Patients are advised to wear elastic support stockings during the day for the first four to six weeks after surgery and to keep their leg elevated when sitting. This swelling usually resolves after about six to eight weeks. Healing of the breastbone takes about six weeks and is the primary limitation in recovering from CABG surgery. Patients are advised not to lift anything more than 10 pounds or perform heavy exertion during this healing period. They are also advised not to drive for the first four weeks to avoid any injury to the chest. Patients can return to normal sexual activity as long as they minimize positions that put significant weight on the chest or upper arms. Return to work usually occurs after the six week recovery, but may be much sooner for non-strenuous employment.
Overall mortality related to CABG is 3-4%. During and shortly after CABG surgery, heart attacks occur in 5 to 10% of patients and are the main cause of death. About 5% of patients require exploration because of bleeding. This second surgery increases the risk of chest infection and lung complications. Stroke occurs in 1-2%, primarily in elderly patients. Mortality and complications increase with:
- age (older than 70 years),
- poor heart muscle function,
- disease obstructing the left main coronary artery,
- diabetes,
- chronic lung disease, and
- chronic kidney failure.
